- TuneUp Utilities 2012: Get your PC in top shape! The PC optimization workout. More than 30 tools guarantee PCs maintain peak performance when working, playing, and gaming. Full hard disk and registry clean-up included.
- Tuneup Utilities Free Download; Tuneup Utilities Windows 10; If you are serious about milling with an Alaskan mill, this is the ultimate set-up. This kit includes everything you will need to cut large slabs with ease, and it allows you to hook up two powerheads for ultimate ripping power (50' cuts through hardwood go a lot faster with two saws pulling for you!).
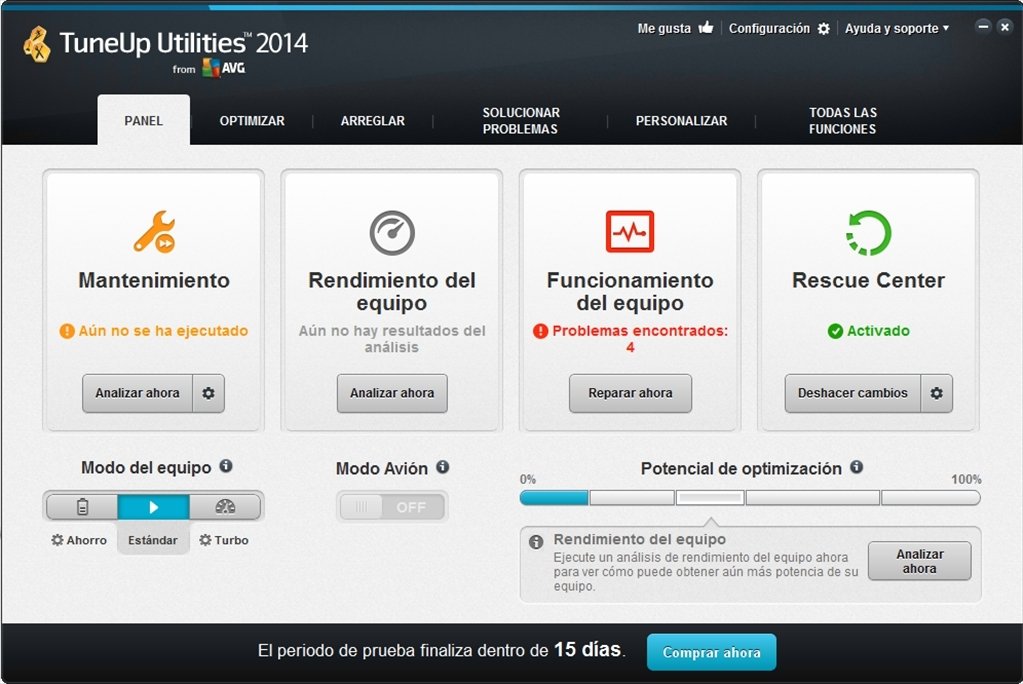
- AVG TuneUp speeds up and cleans your PC by scanning for, then allowing you to safely remove unnecessary files from your system. AVG TuneUp also scans for issues that can cause system crashes and unpredictable behavior, including unnecessary programs installed on your PC, out-dated software, and unusual system settings.
- TuneUp Utilities is an interesting application with the only goal of tuning up your PC. Increase performance, free-up Disk-space, Maintain Windows, Solve problems, Customize Windows and the rest of tools in a group all together. Defragment the Hard Drive, accelerate Internet and Windows itself, eliminate junk data, clean up the registry, solve.
TuneUp Utilities, 2013, Portable, Free Download, Full Version, Portable Download, PC Softwares, Pc Tunning Softwares.
Tune Up Utilities 2012 Portable Hot Hidden Express Game Shree Serial Song Download News: Pilotedge Receiver Now Available For Mac Volvo Vida 2012a Rapidshare Search Works Of Satoshi Kamiya 3 Pdf 64-bit Version Of Dpinst.exe Download Lagu As Long As You Love Me Mp3 Programmers: Conio.h's Kbhit Equivalent For Mac.
AVG PC TuneUp is a free utility that sweeps away junk files, frees up disk space, and keeps itself up-to-date. For an in-depth review of TuneUp Utilities, please refer to our AVG PC TuneUp page. Download tuneup utilities 2012 2012 12.0.2160.11, tuneup utilities 2012 2012 12.0.2160.11, tuneup utilities 2012 2012 12.0.2160.11 download free.Missing.
The third-generation M-Audio Oxygen 49 ($189.95 list) is a solid 49-key MIDI keyboard controller that works with PCs and Macs. It's actually part of a four-product lineup, which consists of the Oxygen 25, the Oxygen 49, the Oxygen 61, and the Oxygen 88, with each number reflecting the corresponding key bed size. It turns out that regardless of which one you choose, the M-Audio Oxygen is an easy Editors' Choice. It offers excellent value as a day-to-day controller for ($14.99, 4.5 stars), as well as pro-level digital audio workstations, virtual synthesizer plug-ins, and music instruction software. Design and Controls The Oxygen 49 measures 29 by 9.4 by 3.7 inches (HWD) and weighs 6.4 pounds. The keyboard is made entirely of plastic, with a smooth, expensive-looking gray finish, and full size ivory-like keys.
It looks bluish in photos, but in person it appears gray, and it feels solid and well made. One of the reasons why the M-Audio Oxygen line has been successful for so long is its vast array of MIDI control features, and here the Oxygen 49 doesn't disappoint. Starting at the top left, there are two plastic pitch bend and modulation wheels, each one with a sizable finger indent. Four rubber keys to the right handle Track Select and transposition. To the right of those keys, a 3-digit red LED display shows the currently selected parameter—usually with a range of 0 to 127, although it also shows octave and preset info. This is one place that even a slightly larger LED display would be helpful, though I suppose M-Audio has to save something for its more expensive Axiom line (which also features higher quality, semi-weighted keys and eight drum sample pads, among other upgrades).
The Oxygen 49's back panel, meanwhile, features a standard-size USB port, a sustain pedal jack, and a power switch, with a Kensington-style lock opening on the right side for security purposes in student and educational settings. The Oxygen 49 comes with a six-foot USB cable, but no AC adapter. In fact, there's no DC power jack, either. That's not a problem with today's PCs, but it hampers compatibility with an iPhone or iPad, since third-party MIDI adapters like the (3.5 stars) assume AC power for the keyboard. I wouldn't have minded if the AC adapter was optional, but to remove the jack with it seems a bit excessive. Programming, Performance, and Conclusions A long row of rectangular keys just above the keyboard let you program controller information.
These work in conjunction with the MIDI keyboard itself, which when placed in Edit mode handles various functions according to the labels behind the keys (such as for bank switching, velocity curves, and drawbar programming). More prominently, there are nine assignable sliders in the center of the keyboard, plus eight assignable knobs on the right side. Dedicated transport keys sit on the right beneath the knobs. All of the controls feel good to the touch and move with precision. I tested the M-Audio Oxygen 49 with a custom-built Core i7 PC running (4.5 stars), (4 stars), and (3 stars), as well as with a 15-inch MacBook Pro running (4.5 stars).
The Oxygen 49 worked flawlessly in all cases. Key feel is on the light side, but felt precise enough that I wasn't constantly reminded I was playing a budget-priced controller, and the vast array of knobs and sliders made controlling on-screen parameters a breeze. If you're looking for something that feels more like an actual piano, you'll want semi-weighted or fully weighted, piano-style keys with solid front ends.

Download Tune Up Utilities 2012 Portable Full
The new Oxygen 88 looks like a good alternative, although I haven't tested it yet; there are of course many other 88-key controllers out there. On the smaller side, the (3.5 stars) is a slightly lower-cost alternative that omits most of the controls. The Q25 features a two-inch shallower depth that makes it easier to place on a small desk, although it's a bit wider, as the pitch bend and modulation wheels are on the left of the key bed. If you're planning on using your controller with an iPad, the (3.5 stars) offers a built-in slot to sit the tablet neatly in front of you and at an angle, although it lacks the Oxygen 49's copious array of assignable sliders, knobs, and transport controls and doesn't feel quite as robust.
More Audio Accessory Reviews: .
Obstructive sleep apnea (OSA), a syndrome defined by breathing abnormalities during sleep, can lead to fatigue and excessive daytime sleepiness (EDS) with an increased risk of motor vehicle crashes. Identifying commercial motor vehicle operators with unrecognized OSA is a major public health priority. Portable monitors (PMs) are being actively marketed to trucking firms as potentially lower-cost and more accessible alternatives to the reference standard of in-laboratory polysomnography (PSG) in the diagnosis of OSA among commercial motor vehicle operators. Several factors regarding PMs remain uncertain in this unique patient population: their sensitivity and specificity; the cost-benefit ratio of the PMs versus PSG; potential barriers from human factors; and evolving technologic advancement.
Human factors that alter test accuracy are a major concern among commercial drivers motivated to gain/maintain employment. Current available data using PMs as a diagnostic tool among CMV operators indicate relatively high data loss and high loss to follow-up. Loss to follow-up has also been an issue using PSG in commercial motor vehicle operators. Furthermore, PM testing and PM results interpretation protocols may have no sleep specialist oversight, and sometimes minimal physician oversight and involvement.
Additional studies comparing unattended and unmonitored PMs directly against full in-laboratory PSG are needed to provide evidence for their efficacy among commercial motor vehicle operators. BACKGROUND Large commercial motor vehicle crashes are an important public safety hazard in the United States. Since 2003, more than 100,000 injuries and more than 5,000 fatalities in the United States occur each year involving commercial motor vehicles. Among single-vehicle accidents involving heavy trucks, almost 18% of the involved drivers admitted to having fallen asleep behind the wheel and more than 50% of these accidents were determined by investigators to be fatigue-related., Factors causing fatigue among truck drivers include sleep deprivation, poor sleep hygiene, travel, shift work, drugs, alcohol, and sleep medications as well as sleep disorders including the most common, obstructive sleep apnea (OSA). OSA has a high prevalence among commercial motor vehicle operators, and it is known to lead to fatigue and excessive daytime sleepiness (EDS) and to increase the risk of motor vehicle crashes.,– Determining which commercial motor vehicle operators are prone to fatigue and EDS due to OSA is becoming a major public health and trucking industry priority.
The current gold standard for diagnosing OSA is a laboratory-based polysomnography (PSG) study. The in-laboratory PSG is often expensive, time-consuming, and frequently of limited availability. Prevalence OSA is a syndrome characterized by stoppages or reductions in breathing during sleep. Screening Criteria for Commercial Motor Vehicle Operators In this review, the term “screening” is used to describe risk assessment or stratification, namely, the application of questionnaires, body mass index (BMI), blood pressure, neck circumference, or other criteria to all commercial motor vehicle operators to determine which drivers are at higher risk of OSA and would be required to undergo a “diagnostic” procedure for ruling out or ruling in the presence of clinically important OSA. The terms “diagnosis” and “diagnostic” procedures for OSA are used to refer to different types of sleep studies, PMs, or full-channel PSG, which measure or estimate the presence or absence of OSA and the severity of sleep apnea via the apnea-hypopnea index (AHI) or respiratory disturbance index (RDI) or other means.
The only federally mandated screening item for OSA and other sleep disorders during the conduct of commercial drivers medical examinations (CDME) is a single, driver-answered question on the FMCSA's medical examination form. The question asks drivers whether they have: “Sleep disorders, pauses in breathing while asleep, daytime sleepiness, loud snoring.” Unfortunately, almost all drivers, even those at high risk of OSA or with known OSA diagnoses, answer this question negatively. Famous pieces written for piano. The 2008 recommendations made to the FMCSA thus far have not been implemented as requirements. Barriers to a federal mandate stem from politics, finances, liability, and legal concerns.
Some clinics have lost clients because they have voluntarily implemented screening guidelines in their commercial drivers medical examinations. At least four sets of recommendations exist for screening commercial motor vehicle operators: the FMCSA Medical Expert Panel, the FMCSA Medical Review Board, the Joint Task Force, and the study by Dagan et al. The FMCSA Medical Expert Panel consisted of experienced clinicians and researchers knowledgeable in evidence-based medicine. The 2008 report of the Medical Expert Panel recommended referral of all commercial motor vehicle operators with BMI ≤ 33 kg/m 2 for a sleep study based on work by Gurubhagavatula et al. Showing that a BMI of 32.7 kg/m 2 is the optimal cutoff point to identify OSA with a sensitivity of 76.9% and specificity of 70.5%., Although a lower BMI would have increased sensitivity, it would have required many more sleep studies.
Therefore, the Medical Expert Panel took feasibility of implementation into consideration and aimed to identify most commercial motor vehicle operators with severe OSA. Ultimately, the FMCSA Medical Review Board recommended a lower BMI criterion (BMI ≤ 30 kg/m 2) after reviewing all the negative long-term medical outcomes from untreated OSA. Used a BMI ≤ 32 kg/m 2 as a screening criterion for PSG referral, which identified 77% of these drivers with BMI ≤ 32 kg/m 2 as having OSA. Also found no correlation between the drivers' subjective reports and objective findings.
All of the drivers denied sleep complaints and EDS. The 2006 Consensus Conference Criteria or Joint Task Force of the American College of Chest Physicians, American College of Occupational and Environmental Medicine, and the National Sleep Foundation issued recommendations for OSA screening among commercial drivers at certification examinations by commercial drivers medical examinations., Their screening recommendations include self-reported historical findings and the Epworth Sleepiness Scale (ESS), but emphasized objective physical examination findings such as BMI, neck circumference, and hypertension criteria. The Joint Task Force guidelines recommended a higher BMI threshold (BMI ≤ 35 km/m 2) for sleep study referral, designed to have a high positive predictive value and identify more severe OSA cases while not removing too many drivers from service.
Subsequent studies demonstrated that the Joint Task Force criteria had a very high positive predictive value for OSA case finding exceeding 90%., However, based on OSA prevalence estimates of 12-13% in driver populations derived from those cases identified by the Joint Task Force guidelines, the sensitivity of the Joint Task Force may only approach 50%. Estimated OSA prevalence and positive predictive values in current guidelines, recommendations, and data Although most occupational physicians agree that screening commercial drivers for OSA is important, most do not conduct OSA screening of drivers according to the Joint Task Force or other rigorous recommendations. Additional education and dissemination of information regarding OSA, its effects on drivers, and the utility and accuracy of various screening methods are needed. The lack of a federal mandate and the ability of drivers to seek out examiners who provide less rigorous commercial driver medical examinations (“doctor shopping”) are major obstacles in implementing OSA screening. As long as there are a lack of federal rules mandating rigorous OSA screening, cursory examinations and “doctor shopping” will likely continue, compromising OSA case finding and, ultimately, driver health and public safety. A recent cost analysis showed that OSA screening of drivers would be cost-effective provided that diagnosed cases had high treatment adherence. Arguably, a regulatory mandate that included a requirement for diagnosed cases to demonstrate treatment compliance would improve case finding as well as treatment adherence.

Unique Behavior of Commercial Motor Vehicle Operators in the Context of OSA Screening Screening for OSA in an occupational setting creates multiple challenges. For example, the timing of the sleep study (whether to do it before employment or after employment) can influence who is responsible for payment of the sleep study and related costs. Some drivers lack insurance before being hired. The waiting time to testing and treatment can be long and can result in temporary removal of the employees from their duties. These factors pose potential economic loss for the employees and financial and staffing issues for the employer.
Additionally, unlike the typical setting in a sleep clinic where patients with undiagnosed OSA are actively seeking diagnosis and treatment for inadequate sleep, snoring, and/or EDS, most commercial motor vehicle drivers actively avoid an OSA diagnosis because of its economic and occupational implications. Thus, relying on self-reported symptoms by commercial drivers during screening for OSA and other sleep disorders has been challenging and of very low yield in occupational settings., In fact, commercial drivers often do not report any symptoms, medications, or diagnoses at driver certification examinations. Found that 85% of drivers with likely OSA answered negatively to the federally mandated question about “Sleep disorders, pauses in breathing while asleep, daytime sleepiness, loud snoring.” Furthermore, the same study found that some drivers with previously diagnosed OSA initially denied the presence of a sleep disorder until they were told that based on screening criteria they were required to obtain a sleep study. In another example, a 2006 study in Israel showed 78% of its commercial drivers with BMI ≥ 32 kg/m 2 had PSG-confirmed OSA and almost half also had objectively confirmed EDS as measured by a multiple sleep latency test. However, 100% of these affected drivers denied symptoms of OSA or EDS. Likewise, most OSA-affected CMV operators report very low ESS scores at driver certification examinations (range 2-4), which are markedly lower than ESS scores from the general community. Further complicating the picture, in the absence of employer-mandated programs, 33-67% of those who are identified as high risk for OSA according to Joint Task Force criteria often either do not complete a full laboratory PSG due to lack of insurance or “doctor-shopping.”, With “doctor-shopping,” drivers seek an alternate commercial driver medical examiner who is not familiar with formal OSA screening recommendations or otherwise does not screen for OSA using objective criteria.
In some cases, such behavior has led to fraudulent certification (for example, the driver is not forthcoming with the medical examiner about OSA diagnosis) followed by an at-fault motor vehicle crash and eventual criminal prosecution of the operator. Although the FMCSA is in the process of establishing a National Registry of Certified Medical Examiners program that would require medical examiners receive training and pass a minimum competency certification test before being listed as an authorized medical examiner to conduct the commercial motor vehicle driver physical examination, the Registry will not collect the fully completed examination forms and the willingness and ability of drivers to doctor-shop may continue. The availability of medical examiners who are not rigorous is supported by a recent Government Accountability Office report. This report found that many commercial motor vehicle operators with serious health conditions rendering them eligible for government disability benefits are somehow still able to obtain medical certification for commercial drivers' licenses, implying paradoxically that they are physically fit to drive large vehicles.
Additional evidence of this problem came from a 2009 survey of occupational medicine providers, which documented a fear of losing clients and doctor-shopping as a major obstacle to more widespread OSA screening of commercial motor vehicle drivers. CURRENT GUIDELINES FOR DIAGNOSTIC STRATEGIES FOR CONFIRMING OSA IN COMMERCIAL MOTOR VEHICLE OPERATORS Once a high-risk commercial motor vehicle operator is identified at a commercial drivers medical examination, an accurate characterization of the presence or absence of OSA, and if present, severity of OSA becomes important to choose an appropriate disease management plan. The gold standard test for diagnosing and determining the severity of OSA is still in-laboratory, technician-monitored PSG. The definition of OSA currently involves the measured AHI or the average number of apnea and hypopnea episodes over one hour. RDI has also been used as an alternative scale for those measures. An apnea is defined by AASM as cessation (defined as 90% reduction) of air movement lasting more than 10 sec.
Apnea can be distinguished from hypopnea (defined as 50-90% decrease in air flow) via a thermistor in PSGs (hypopneas are detected via a nasal transducer), although the consequences of hypopneas versus apneas are generally thought to be similar. Although the definition of apnea has been uniform, three different criteria to score hypopnea are in common use: the AASM recommended criteria, AASM alternative criteria, and the Chicago Criteria. Sleep laboratories may use different criteria for scoring, and the resultant AHIs would vary considerably.
Thus, the variable technology and criteria used for assessing respiratory disturbance during sleep represents a challenge for the field. The 2006 Joint Task Force Guideline recommends that all commercial motor vehicle operators who are suspected of having OSA at the commercial driver medical examination be assessed by a sleep specialist and have a confirmatory diagnosis by PSG. Since that time, there has been an increase in demand for access to sleep laboratories.
However, there are major factors that limit access to appropriate testing and timely diagnosis. PMs offer an alternative lower upfront cost strategy (at least in theory) to PSG. The AASM published clinical guidelines in 2007 for the use of unattended PMs in the diagnosis of OSA. It recommended that unattended PMs be used only (1) in conjunction with a comprehensive sleep evaluation, supervised by a practitioner with qualifications for certification in sleep medicine; (2) in patients with a high pretest probability of moderate to severe OSA and without other comorbid medical or sleep conditions; (3) in patients for whom in-laboratory PSG is not possible due to immobility, safety, or critical illness; and (4) to monitor the response to noncontinuous positive airway pressure treatment for OSA. In the setting of an occupational clinic overseeing commercial driver medical examinations, a sleep medicine specialist is almost never available on site at the time of these examinations. Furthermore, defining high pretest probability is often hampered by the unique behaviors of the commercial motor vehicle operator population described earlier.
Tuneup Utilities Crack
Comorbid medical conditions or other sleep conditions among commercial motor vehicle operators frequently exist (for example, hypertension, diabetes mellitus, chronic obstructive pulmonary disease, congestive heart failure, or circadian rhythm sleep disorders). However, in contrast with AASM guidelines, in practice some testing companies are directly marketing PM-based strategies to trucking firms as potentially appropriate for testing any driver for the presence of OSA, whether or not that driver is at high risk for OSA with high pretest probabilities of OSA. Second, trucking firms are sometimes being given the impression that high-risk OSA drivers with negative PM studies do not require further in-laboratory testing. Third, PM testing and PM results interpretation protocols may have no sleep specialist oversight, and sometimes minimal physician oversight and involvement. In 2008, the expert panel and medical advisory board to the FMCSA recommended that the preferred method of diagnosis and assessment of OSA be an overnight PSG, but “acceptable alternative methods for assessment of risk in CMV commercial motor vehicle drivers include objective recording devices, validated against PSG, that include at least 5 h of measurements of oxygen saturation, nasal pressure and sleep/wake time.” In the same year, the US Centers for Medicare and Medicaid Services (CMS) approved reimbursement for the use of PMs.
Free Trial Tuneup Utilities
The approval is partially due to the mostly positive review of PMs by the Agency for Health Quality Research, which pointed out that PMs have comparable clinical utility to predict clinical outcomes in a population with high pretest probability for OSA., For the purposes of diagnosis, titration of continuous positive airway pressure, and continuous positive airway pressure adherence, PMs and laboratory-based PSG have equivalent functional outcomes among the high pretest probability population. TYPES OF PMs OR LIMITED CHANNEL TESTING The AASM has classified sleep studies into four types, depending on the channels they record and evaluate. A new classification for PMs called the SCOPER (Sleep, Cardiovascular, Oximetry, Position, Effort, and Respiratory) system has been recently proposed; however, many of the important issues for determining pretest probability, interpreting study results, and developing testing algorithms and treatment decisions are still under way. For the purposes of this review paper, we use the pre-SCOPER system definition to maintain consistency with existing literature. Type I PSG serves as a reference standard PSG.
It is a nocturnal, technician-attended, full in-laboratory sleep study with 14-16 channel monitoring. A type I PSG assesses numerous physiologic parameters. A type II PSG records the same information as a type I PSG but lacks technician attendance and may be done in or out of the laboratory setting. The Sleep Heart Health Study, a large multicenter trial, was done by type II portable monitoring at home. Four types of PSG currently classified by the American Academy of Sleep Medicine and novel devices Most of the so-called PMs being used for home diagnosis of OSA are type III and type IV. Type III PM includes oximetry, at least two respiratory channels (two airflow channels or one airflow plus one respiratory effort channel) and electrocardiogram-monitored heart rate, but it usually does not include electroencephalogram, electromyogram, and electro-oculogram. As a result, signals used to detect sleep/wake stages and arousals from sleep in type I and II are lacking in type III PM.
An obvious shortfall of type III PMs is that, without sleep/wake assessment a true AHI or sleep efficiency cannot be obtained. Most PMs report only RDI defined by respiratory events divided by total recording time (versus sleep time).
Download Tune Up Utilities 2012 Portable Free
Given that PMs generally use recording time rather than total sleep time, RDI from PM tends to underestimate the severity of sleep apnea than AHI from PSG. Another common problem of using PMs on commercial motor vehicle operators is that without documenting sleep, an individual could wear the device (or give it to someone else) and deliberately stay awake, yielding a falsely low RDI. Furthermore, it is important to mention that RDIs of different type III PMs vary with different device manufacturers. The scoring method of PMs is not currently standardized by AASM, resulting in RDIs difficult to compare across different studies of portable devices. The inability to detect respiratory effort related arousals can also lead to underestimation of the RDI and underrecognition of upper airway resistance syndrome. Type IV PMs share at least the same shortcomings of type III PM, and the current CMS guidelines require a minimum of three channels to meet the reimbursement criteria. However, we emphasize here the sensitivity and specificity of the various diagnostic techniques rather than the number of channels per se.
Download Tune Up Utilities 2012 Portable Usb
In addition to the conventional PM classifications discussed in the previous paragraphs, recently published data on new technologies such as combined actigraphy, oximetry, and peripheral arterial tonometry (without detection for airflow) may theoretically improve diagnostic accuracy of portable monitors for OSA and the estimation of sleep stages.,– However, the accuracy of this sleep staging technology is modest at best, leading to a challenge to improve technology with new, simple devices. Other technologies measuring forehead venous pressure and venous volume have been used to estimate respiratory effort., As mentioned previously, a new classification of PM has been recently proposed and will likely evolve depending on the technology available. In addition to the evolving technologies, there are several ways to score apnea and hypopnea events in PMs: manually by a technologist or sleep physician, automatically by the software of the PMs, or combined (manual correction on the automated scoring). However, automatic scoring so far has not proven sufficiently accurate when compared to manual scoring, although efforts are clearly ongoing.,– There is also evidence that oximetry seems to be the most predictive component for assessment of OSA, regardless of using PMs or laboratory-based PSG. However, to date, no model or psychometric instrument has been shown to stratify accurately individuals with OSA by disease severity. ADVANTAGES AND DISADVANTAGES OF PM FOR COMMERCIAL MOTOR VEHICLE OPERATORS Given the unique behavior of commercial motor vehicle operators described earlier and that most PMs do not measure sleep/wake stages, the potential for sabotaging or gaming the results of PMs by commercial motor vehicle operators remain a likely possibility (commercial motor vehicle operators may choose to stay awake all night to avoid respiratory events). In a second scenario for data fudging, unless the PM device has “chain of custody” and is placed by a professional on the subject, drivers may place the device on a healthier family member to avoid an accurate diagnosis.
Given the known “doctor shopping” tendency reported in many commercial motor vehicle operators, it is also appropriate to suspect that the sensitivity for OSA diagnosis using type III or type IV PMs will be lower than that done in the general population. Furthermore, most published reports comparing PMs with PSGs use less sensitive cutoff definitions for diagnosing sleep apnea: typically an RDI or AHI of ≥ 15 or even ≥ 30/hr. It is not clear at this point that untreated mild OSA does not increase crash risk. Other disadvantages of PMs include absence of a trained technologist to correct and clarify artifacts and make ongoing equipment adjustment during testing, inability to intervene in medically unstable patients, potential data loss or distortion, potential for misinterpretation of the results due to limited data, lack of a standard protocol, and a lack of standards for scoring. Compounding these deficiencies, some of the strategies being marketed to trucking companies lack sleep specialist involvement, which potentially leaves the interpretation of PM data up to occupational health and primary care providers who may be unaware of the technology's limitations. For example, it is doubtful that most drivers at high risk of OSA with negative PM tests are being referred for a subsequent in-laboratory type I PSG in agreement with current guidelines.
On the other hand, potential advantages of PMs include increased accessibility, easier setup, and lower up-front cost. Additionally, PMs have the advantage of allowing the subject to sleep at home or another familiar environment.
Most normal sleepers can experience transient insomnia (or some degree of sleep disruption) the first time they sleep in the unfamiliar environment of a laboratory. This so-called “first night” effect associated with in-laboratory PSG may result in a less accurate picture of the subject's usual sleep patterns. CURRENT EXPERIENCE WITH PMs As mentioned earlier, the medical expert panel for FMCSA in 2008 recommended that PSG be used as the preferred method of diagnosing OSA, and PMs as an alternative diagnostic tool must be validated against PSG and include oximetry, nasal pressure, and sleep/wake time.
No study to date has appropriately validated the applicability of devices meeting those criteria against PSG in commercial motor vehicle drivers. Current data showing relatively low sensitivity and specificity of PMs remain a challenge for large-scale screening and diagnosis of OSA among commercial motor vehicle operators. Further prospective randomized studies conducted in collaboration with both trucking employers and academic sleep centers in direct comparison with various PMs and type I PSGs will be important.
The legal ramifications for commercial motor vehicle operator and employers remain uncertain. There are currently no regulations specifying the qualifications of health care providers using PM testing, nor any standards specifying the “best” PM technologies.
Tuneup Utilities free. download full
Download Tune Up Utilities 2012 Portable Pc
For example, the practice guidelines for PM testing from AASM specify direct measurements of airflow and respiratory effort; however, many PM technologies are proprietary methods that derive these values indirectly from other directly measured parameters., The deployment of PMs frequently do not involve board certified sleep specialists, and reading and interpreting the studies are often automatically scored on site, potentially compromising the diagnostic accuracy of the disease. Furthermore, published PM studies generally required two nights of PM. The testing results for OSA are sometimes not independent of the medical equipment provider, resulting in potential conflict of interest.
The conservative estimation of the overall sensitivity of PMs done between 1996 and 2009 is approximately 90% and specificity is at best approximately 80%. In other words, in approximately 10% of the commercial motor vehicle operators screened, a diagnosis will not be picked up by the PMs; approximately 20% of the commercial motor vehicle operators screened will be given a false diagnosis of OSA by the PMs. Additionally, available studies estimate approximately 12% data loss and 8% data fudging. Thus, more recordings may often be required. To illustrate what would happen when 100 high-risk commercial motor vehicle operators use PMs for the diagnosis of OSA we have constructed a schematic flowchart. In this scenario, as many as 42 of the 100 commercial motor vehicle operators who initially undergo PM studies may require in-laboratory PSGs in the end, due to either data loss, data fudging, or negative PM study results.
Potential applicability of portable monitors (PM) in 100 high-risk commercial motor vehicle operators. To date, the only peer-reviewed, published study using PMs to diagnose OSA in the US CMV population was by Watkins et al. The study uses RUSleeping RTS, a single-channel device (type IV PM) that measures airflow (nasal pressure) by a nasal cannula and estimates RDI. Of those commercial motor vehicle operators presenting for a commercial drivers medical examination who met 2006 Joint Task Force OSA Consensus Conference Criteria (n = 109) for high risk of OSA, 68 (62%) were randomly selected to use donated RUSleeping™ RTS PM device for one night at a certified community sleep center under the supervision of sleep physicians and undergo a subsequent formal PSG in the laboratory. Twenty-two percent of the randomized commercial motor vehicle operators who met the Joint Task Force criteria for PSG were lost to follow-up.
Among the remaining drivers who underwent PM, as many as 49% of the drivers were noncompliant with physician recommendations and were therefore not able to complete the subsequent PSG. Sixteen percent of drivers using the PM test produced invalid data for a variety of reasons.
Given these results from a study done at a certified community sleep center, it is reasonable to postulate that incidents of data loss and alteration will likely be as high or higher when they are used on commercial motor vehicle operators in unsupervised home settings or on the road. Large prospective studies comparing type III PM against full in-laboratory PSG in a large commercial motor vehicle operator population are desirable to provide definitive evidence for the validity of PMs in diagnosing OSA among commercial motor vehicle operators. COST BENEFITS OF PM VERSUS PSG The cost benefits of PMs are controversial.
The relatively high false-negative rate along with the current guideline that all negative PM tests in patients with a high pretest probability of OSA should be referred to a full in-laboratory PSG by a sleep specialist may translate into an overall higher cost if the currently available PMs were to become the mainstream of screening tools among commercial motor vehicle operators and guidelines were followed. Have recently provided a theoretical framework to ascertain the pretest disease probability above which portable studies would be economically attractive as an initial test in the assessment of suspected OSA among CMV operators. Likewise, Pietzsch et al. Have applied decision analysis and the Markov model to conclude that there is a lifelong cost effectiveness using PSG (versus PMs) in diagnosis and treatment of moderate to severe OSA, assuming a population with 50% prevalence for OSA. It is important to recognize that the end results of all economic modeling studies depend heavily on the underlying assumptions and data applied by the model.
No study or model to date has adequately assessed the cost effectiveness of a PM-based strategy among commercial drivers. CONCLUSION Compared with the gold standard of type I PSG, PMs have begun to gain more attention among primary care physicians, occupational clinicians, insurers, the trucking industry, and patients as an alternative means of diagnosing OSA. However, commercial motor vehicle operators have unique and well-described behaviors during the process of commercial driver medical examinations that are likely to make the proper use of PMs more challenging and lower yield than among the general population.
These factors make it unwise to directly extrapolate PM efficiency and cost-effectiveness assumptions from the general population to the professional driver population. Further research conducted in the trucking industry is needed to determine the utility of PMs and best practices for their use in diagnosing OSA among commercial motor vehicle operators. DISCLOSURE STATEMENT Dr. Zhang has no financial support from any for-profit agencies. Berger is a CEO and chief medical officer for Precision Pulmonary Diagnostics, is a private for-profit company that provides sleep apnea-related services to commercial trucking companies. Kales has served as a medicolegal consultant and expert witness on cases involving commercial drivers and has consulted with Circadies. Malhotra has consulting and/or research income from the National Institutes of Health, American Hospital Association, Philips, SGS, Sleep HealthCenters, and Apnex.
No conflict of interest is known.